Manual prescription often leads to administrative burdens and increased risks of medication errors, which can adversely affect patient safety. To address these issues, managed care pharmacists introduced electronic prescribing, the electronic generation and transmission of prescription orders between healthcare providers and pharmacies.
Despite its benefits, adoption has been slow, with only 7% of medical doctors prescribing medication through their electronic medical records (EMR) software. With growing e-prescribing standards tied to incentives, more healthcare practitioners opted to adopt EMRs that feature e-prescribing.
This blog explores the transition from traditional paper-based prescriptions to digital systems and how this shift positively impacts patient safety in the healthcare ecosystem.
What is Electronic Prescribing?
E-prescribing is a secure method that allows healthcare providers or prescribers to electronically access the health plan formulary, eligibility of patients, and their medication history at the point of care.
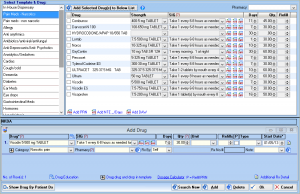
In the past, e-prescribing involved data entry and faxing. Nowadays, e-prescribing has evolved into a comprehensive application that offers a secure connection between pharmacies and various healthcare settings. Here’s a list of its different functionalities:
- E-prescribing software can flag potential drug interactions, allergies, or dosage discrepancies.
- EMR with integrated e-prescribing facilitates seamless communication between healthcare providers and pharmacies.
- E-prescribing eliminates handwriting-induced errors by providing typed, precise prescriptions.
- Some advanced EMR software with e-prescribing can support patient adherence by providing reminders and educational resources.
- EMRs offer a comprehensive view of a patient’s medication history.
The integration of e-prescribing within EMR systems represents a significant leap forward in patient safety. As of 2021, e-prescriptions accounted for 94% of all prescriptions filled, demonstrating the effectiveness of this innovative system.
How E-Prescribing Integration Helps With Patient Safety
E-prescribing has proven to be a game changer in mitigating traditional risks associated with manual prescription processes. By adopting this technology, healthcare providers can deliver efficient and secure care, improving patient outcomes.
Some eprescribing benefits consist of the following:
Reduction in Medication Errors
Electronic systems can flag potential drug interactions, allergies, or dosage discrepancies. This ensures that healthcare providers make informed decisions that enhance patient safety.
Improved Accuracy in Prescription Management
Illegible handwriting on paper prescriptions is a known source of errors. E-prescribing eliminates this issue through clear prescriptions and helps pharmacists accurately interpret and dispense medications.
EMRs with integrated electronic prescribing systems facilitate real-time information exchange between prescribers and pharmacies. This approach streamlines the prescription fulfillment process, contributing to timely medication dispensing.
Enhanced Patient Compliance and Education
Some advanced EMR systems with e-prescribing functionality can support patient adherence by providing reminders and educational resources. This feature fosters patient engagement and helps individuals stay on track with their prescribed medications, ultimately improving health outcomes.
E-prescribing aligns with evolving healthcare regulations and standards. EMR systems with robust e-prescribing capabilities ensure compliance with guidelines related to prescription documentation, tracking, and reporting.
Other Benefits of E-Prescribing
One of the benefits of e-prescribing involves its digital nature and potential for data collection. Practices can leverage analytics to identify patterns, trends, and potential areas for improvement in prescribing practices.
Integrating electronic prescriptions into the billing system or EHR frees up staff time, allowing them to address other tasks. From the patient’s perspective, they may enjoy the convenience of not traveling or waiting in line to leave their paper prescriptions in pharmacies.
How Does E-Prescribing in EMR Systems Work?
E-prescribing in EMR or EHR software involves the digital creation, transmission, and management of prescription orders. Healthcare providers use electronic interfaces within the software to enter patient prescription details, which are then securely sent to pharmacies.
The system often includes the following features:
Prescription Drug Monitoring Program
A Prescription Drug Monitoring Program (PDMP) in EMR systems is designed to track and manage controlled substance prescriptions. It involves the integration of a database that collects and stores information on dispensed medications.
Data Retrieval: The PDMP retrieves real-time data from pharmacies, allowing providers to view a patient’s recent prescription records. This includes medication, dosage, prescribing physician, and dispensing pharmacy. Integrated with PDMP, the EMR may offer clinical decision support features, flagging potential concerns, such as duplicative therapies or signs of substance misuse.
Enhanced Care: PDMP fosters better care coordination by providing a comprehensive view of a patient’s controlled substance prescriptions. This helps identify potential risks, prevent overprescribing, and support appropriate pain management.
Electronic Prescribing for Controlled Substances
Electronic prescribing for controlled substances (EPCS) employs multi-factor authentication and identity verification to ensure that only authorized healthcare providers can prescribe controlled substances electronically.
Preventing Fraud: EPCS helps combat prescription fraud and diversion by eliminating paper prescriptions that can be easily forged or stolen. The electronic format, coupled with secure authentication, reduces the potential for misuse of controlled substance prescriptions.
Secure Transmission: The functionality ensures the secure transmission of electronic prescriptions to pharmacies. Encryption and other security protocols safeguard the transmission process, reducing the risk of interception or tampering.
Medication History
Integrated e-prescribing systems within EMRs provide a complete view of the patient’s medication history. Healthcare providers can access historical information during every visit, providing insights into the patient’s medication adherence, response to drugs, and any prior problems with specific medications.
Patient Engagement: Patients can also access their medication history through patient portals, fostering engagement and allowing them to verify the accuracy of their records.
Automatic Updates: Medication history is automatically updated whenever a new prescription is filled, changes (dosages or start/stop dates) are made to the patient’s medication regimen, or when Electronic Prior Authorization (ePA) processes are initiated.
Drug-to-Drug Interaction Alerts
When a healthcare provider enters a new prescription into the EMR system, the software automatically checks for potential drug interactions based on the patient’s medication history.
Database Access: The EMR system accesses a vast drug database that includes information about potential interactions between medications. Suppose the system identifies a possible drug-to-drug interaction. In that case, it generates a real-time alert for the healthcare provider, which may consist of details about potential risks and recommended actions.
Drug-to-Allergy Interaction Alerts
When a healthcare provider enters an EMR prescription into the system, it automatically checks the patient’s allergies for potential drug-to-allergy interactions. If there is a possible interaction, the system alerts the provider.
Clinical Decision Support: The healthcare provider could also receive guidance on how to proceed, such as selecting an alternative medication safe for the patient’s known allergies or adjusting the dosage to minimize the risk.
Medication Database
When a healthcare provider prescribes medication in the EMR system, the software automatically accesses the medication database to perform safety checks. It compares the prescribed medication with the patient’s medical history, allergies, and current medications.
Documentation: The medication database stores and updates information on various medications, ensuring that healthcare providers can access the most current and accurate data.
Takeaway
Integrating electronic prescribing within EMR systems is a pivotal advancement in healthcare, addressing challenges associated with manual prescriptions. Beyond streamlining administrative tasks, it significantly enhances patient safety by leveraging drug-to-drug interaction alerts, allergy checks, and medication history tracking.
Choose the Top EMR/EHR Software
Experience the next level of patient safety with IMS—a total practice management solution equipped with a powerful e-prescriptions module. Seamlessly integrated into our software, this module manages prescription information and enhances your safety protocols.
Call 480-782-1116 today to schedule a complimentary software demonstration.