EMR & EHR Electronic Claims Processing
For over 10 years, IMS has assisted thousands of healthcare professionals operate their claims and billing more efficiently. Its integrated claims handling is built with an emphasis on improving workflow.Designed to use the latest technologies, our software helps medical practices increase yearly revenues, decrease wasteful spending, and reduce expensive overhead costs. We make claims processing quick and easy so that you and your staff can spend time focusing on patient care.
With IMS, claims are scrubbed in detail before batching. Our software finds if any data is missing, and it reports back both the patient's name and which data is missing. It even allows you to fix the missing data from the same screen.
IMS Integration and Validations - Features
IMS' seamless claims and billing integration allows for faster and more accurate data entry. Some of the features of our software include:
- Automated data entry from electronic medical record superbills
- Strong validations that prevent rejected claims due to missing/incorrect data
- Pre-checking of EMC, CMS-1500 or UB04 claims
- Automatic reconciliation (ERA)
- Enhanced collections and extensive reports to help you keep finances on-track
ICD-10 Ready Electronic Claims Processing Software
Starting on October 1, 2014, all HIPAA-covered healthcare entities will be required to use ICD-10 diagnosis and procedure codes for billing purposes. IMS is ICD-10 ready. Our EHR & Practice Management solutions are fully equipped to meet ICD-10 standards - and we are currently working with healthcare organizations to test that the software can accurately process claims. As part of this process, we test eligibility verification, quality reporting, and other transactions that use ICD-10.


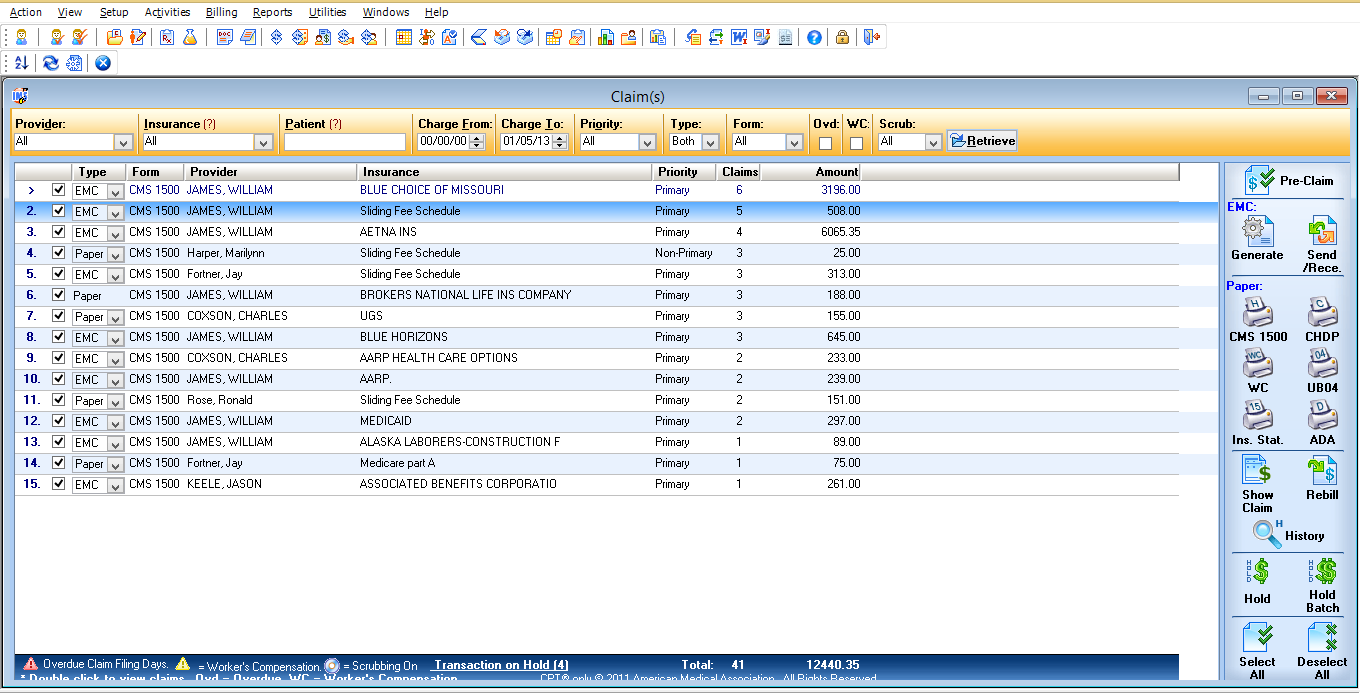
 click to enlarge
click to enlarge