Powerful Insurance Collections Module
 We know that billing and collections are two of the most important and often time-consuming responsibilities for any medical practice. That's why our IMS comes with a built-in, fully-integrated collections module designed to make collections easier and more efficient.
We know that billing and collections are two of the most important and often time-consuming responsibilities for any medical practice. That's why our IMS comes with a built-in, fully-integrated collections module designed to make collections easier and more efficient.
The collections module increases your practice's overall cashflow by streamlining the collections process. The intuitive interface is easy to navigate, greatly reducing errors and inaccuracies.
Our insurance collections module includes:
- An extensive pre-loaded fee schedule
- Pre-loaded specialty-specific templates that are easy to customize to meet your unique needs
- A "Quick Bill" screen that allows users to post charges for all of the electronic superbills with a single click
- A pre-claim analysis that scans claims for missing or erroneous data, sending valid claims and reducing claim rejections
- CMS-1500 templates based on insurance guidelines
- Extensive reports - both built-in and customizable
- Interactive, fully color-coded Patient Ledger
Why Choose Our Collections Module?
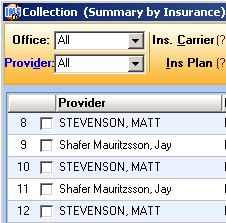
IMS is a powerful billing and collections solution. With IMS' interactive screens, you can click on the column heading and sort the data by that column. This can be handy from the claims screen where you can click on the number of claims column and sort it largest batch to smallest batch. From there, you can drill directly down to the list of all of the patients within that batch, and you can even edit the claims from that screen. IMS allows you to preview the CPT, ICD9 or 10, modifier, units, charge amount, and the entire transaction line. If something is not correct you have the ability to edit it from there.
Insurance Billing Features
- Electronic transmission of patient statements
- True Family Billing
- True Cycle Billing
- True Balance Billing
- Electronic Posting of all insurance payments
- One-click scanning to quickly attach a paper EOB to the payment
IMS also has an amazing feature that allows providers to send patient statements weekly or biweekly. Our highly efficient software will ensure your patients always get their statements on time. There is also a parameter that allows you to tell the software to exclude that patient if a statement has been generated in the last 30 days.
All charges and claims are run through 11 million edits before the claims are sent to the insurance company or clearinghouse.
Special Features to Improve Practice Collections
In addition to its ease-of-use, IMS is also designed to improve your ability to track and process outstanding claims.
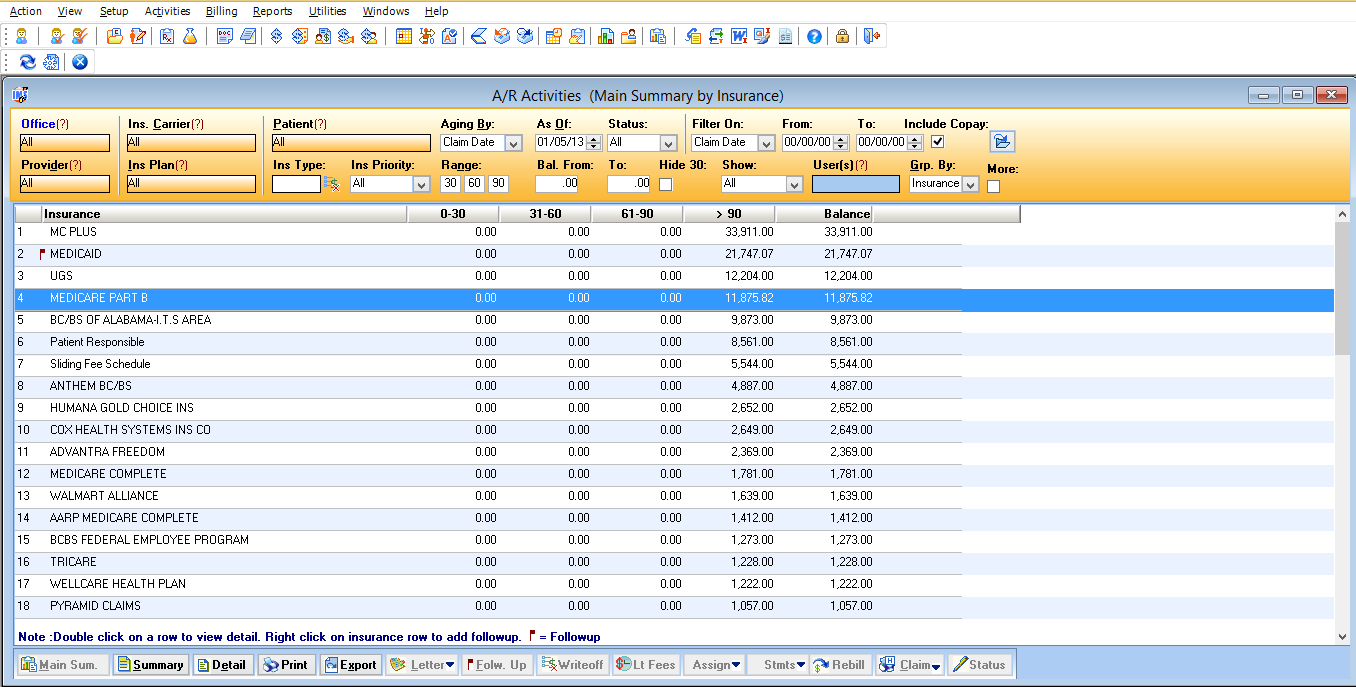
- Provides an interactive aging report
- Tracks unpaid claims using rejection analysis and allows you to easily re-bill claims
- A/R Activity screen identifies top outstanding payers by aging
- Users can easily keep track of their claims with follow-up notes by patient
- Easily analyze outstanding amounts and quickly perform actions from the same screen such as rebilling, write-off, print claims, print statements, etc.
ICD-10 Ready Practice Management Software
Starting on October 1, 2014, all HIPAA-covered healthcare entities will be required to use ICD-10 diagnosis and procedure codes for billing purposes. IMS is ICD-10 ready. Our EHR & Practice Management solutions are fully equipped to meet ICD-10 standards - and we are currently working with healthcare organizations to test that the software can accurately process claims. As part of this process, we test eligibility verification, quality reporting, and other transactions that use ICD-10.


 click to enlarge
click to enlarge