Pre-Claim Checks and Edits
We know that one of the most crucial tasks to the successful operation of your medical practice is an efficient billing system. IMS is designed to streamline the entire billing, claims handling and collections process in one fully-integrated system, making a job that used to take hours simple enough to complete in minutes with fewer errors.
IMS is built to prevent time-consuming errors by providing an intuitive interface that is easy to manage. It also analyzes data for inaccuracies, missing information, duplicate content and incompatibilities. Healthcare professionals have noted a dramatic decrease in rejected claims due to missing and invalid authorization information.
Send Valid Claims The First Time
Our claims scrubbing softawre checks:
- Billing frequency
- Authorization requirements
- CPT codes and diagnosis codes per insurance
- Duplicate entries
- EMC, HCFA or UB92 claims
- Additional data entry errors and missing information
ICD-10 Ready Claims-Checking Software
Starting on October 1, 2014, all HIPAA-covered healthcare entities will be required to use ICD-10 diagnosis and procedure codes for billing purposes. IMS is ICD-10 ready. Our EHR & Practice Management solutions are fully equipped to meet ICD-10 standards - and we are currently working with healthcare organizations to test that the software can accurately process claims. As part of this process, we test eligibility verification, quality reporting, and other transactions that use ICD-10.


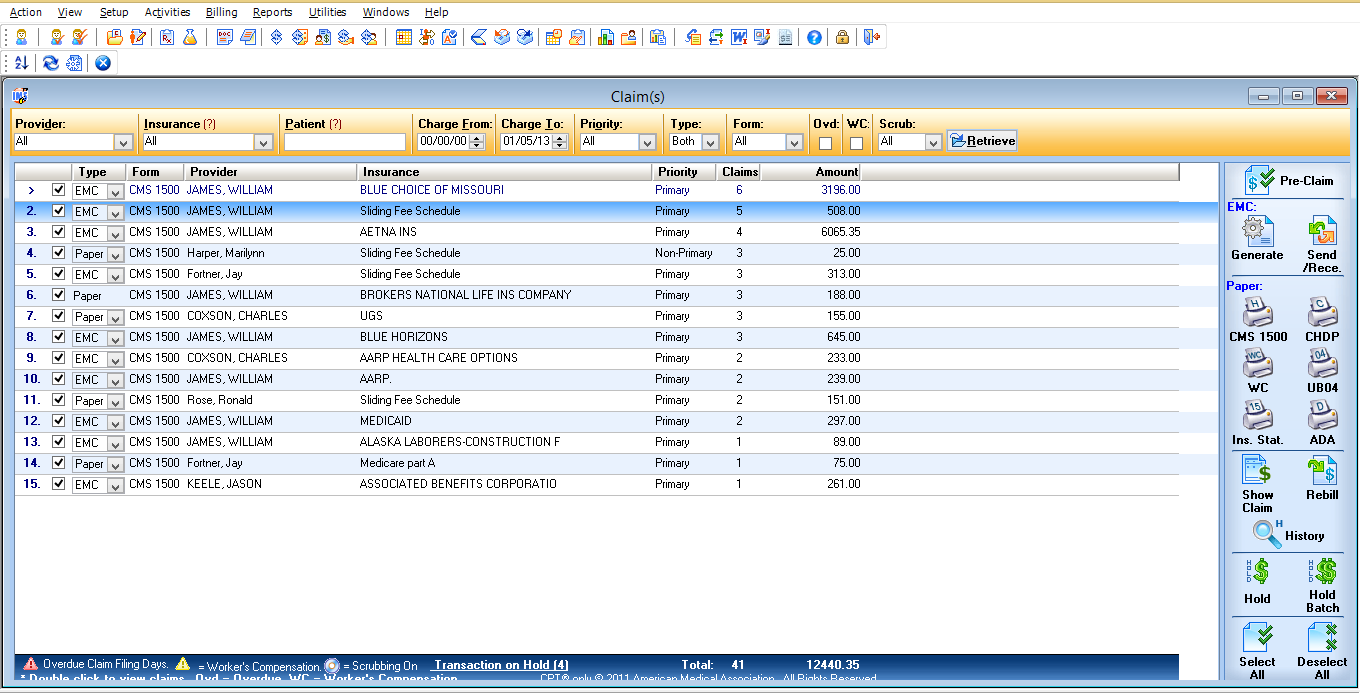
 click to enlarge
click to enlarge